
By: Dr. Angela Di Marco OD, FAAO,
York Finch Eye Associates and Toronto Eye Care
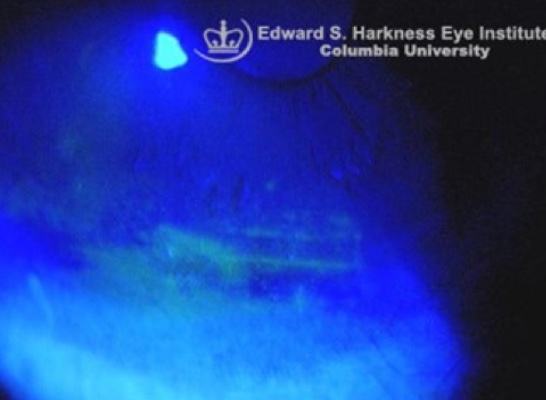
Individuals with acoustic neuromas frequently experience eye discomfort and irritation prior to treatment but, more commonly, following resection of their acoustic neuroma. This is because the facial nerve that is responsible for closing the eye, as well as innervating the lacrimal gland which produces tears, has suffered damage, either temporarily or permanently. As such, individuals may have inadequate tear production (less commonly) and/or may be unable to fully blink and close their eye completely (more commonly) which, in turn, may result in severe corneal dryness. Complete closure of the eye is fundamental to maintain a protected and well-lubricated ocular surface. Resulting corneal dryness from incomplete eyelid closure is aptly named exposure keratopathy. Along with severe pain and discomfort, when left untreated, exposure keratopathy can cause permanent damage to the cornea and sometimes even vision loss.
Fortunately, there are many ways we can treat dry eye disease and exposure keratopathy associated with acoustic neuromas. Management should aim to treat the underlying cause of symptoms whether it be reduced tear production, poor lid function or a combination of both. When treatment is successful, pain and irritation can be minimized, and vision may be improved.
Exposure Keratophy
First-line treatment of dry eye disease and exposure keratopathy secondary to acoustic neuromas often involves the frequent use of preservative free lubricating drops, gels, or ointments (anywhere from four times a day to hourly, depending on the degree of damage) as well as a lubricating overnight ointment along with tape to effectively close the eyelid before sleeping. This prevents the cornea from drying out and protects it during sleep. Moisture chamber goggles provide a similar function and are another popular treatment for both daytime and overnight use but must be fit properly to the eyes. Moisture chamber goggles are an inexpensive tool which can help to maintain moisture on the ocular surface and protect the eye from irritants such as dust, dry air, debris, pollutants etc.
Prescription eye drops that promote tear production, such as Restasis and Xiidra, may help certain patients who suffer from inadequate tear production due to impaired lacrimal gland innervation. Both medications take weeks to months to take effect, and can be expensive; however, oftentimes they can make a positive, non-invasive addition to one’s dry eye treatment regimen. A detailed eye examination can help identify those patients who may benefit from this treatment.
Punctual Occulusion

Punctal occlusion with silicone plugs, or permanent occlusion with cautery, help to prevent tears from draining and thus, keep tears on the ocular surface for longer. This is another common and useful treatment of dry eye disease associated with reduced tear production and exposure keratopathy. A thorough examination of one’s eyelids and one’s tear production can help deduce which patients will benefit most from this treatment. If punctal plugs offer significant improvement to a patient, the punctas may be permanently closed using cautery.
Noctural Lagophthalmos

In some cases, eyelid weights may also be prescribed for patients suffering from incomplete eyelid closure and exposure keratopathy. These weights may be surgically implanted or externally applied to the upper eyelid which uses gravity to assist in the closure of the upper eyelid. In turn, eyelid weights prevent dehydration of the cornea, protecting it from further complications and even loss of vision. A referral to an oculoplastic surgeon is warranted, who will assess the appropriate size and weight that is required.
Scleral Lenses

Therapeutic scleral lenses are another extremely effective tool for patients with severe dry eye disease. Scleral lenses are large, hard contact lenses that sit on the sclera, or the white of the eye. These lenses are very steep and vault the corneal surface leaving the cornea untouched. They are also filled with saline solution prior to insertion. Thus, therapeutic scleral lenses are multi-purpose. They act as a bandage protecting the dry, irritated cornea from exposure to the air while the saline within the lens helps the cornea to heal and provides daylong comfort. Scleral lenses are extremely effective at reducing pain and improving vision for those experiencing severe dry eye disease and exposure keratopathy.
Nevertheless, scleral lenses can be expensive, and insertion and removal of the lenses may be challenging for certain individuals. However, with the right instruction and proper fit, these lenses are a viable long-term daytime solution for patients with chronic corneal dryness.
Oftentimes, the treatment of dry eye disease and exposure keratopathy associated with acoustic neuromas requires more than one solution, and occasionally, what may work for one may not work for another. Thus, it is imperative that a thorough history is taken, and that a detailed eye examination is conducted with your eye doctor. This will help deduce which treatment option(s) is/are most suitable for the degree of symptoms, as well as for the degree of facial nerve damage and corneal involvement.
Angela Di Marco OD, FAAO
Dr. Di Marco further continued her optometric training following graduation from the New England College of Optometry in Boston by completing an Ocular Disease residency at Bascom Palmer Eye Institute in Miami, Florida, consistently ranked as the number one ophthalmology hospital in the United States. There she worked closely with world-renowned ophthalmologists serving various sub-specialty clinics including ocular oncology, cornea, surgical retina, glaucoma, and neuro-ophthalmology. Dr. Di Marco also ran an optometric clinic strictly serving Miami’s underprivileged communities, including drug and alcohol rehabilitation programs, as well as correctional institutions.
She is the Lead Optometrist at York Finch Eye Associates and Associate Optometrist at Toronto Eye Care. She specializes in Ocular Disease including Dry Eye Disease and Myopia Control for children.

