Acoustic neuromas (AN) are benign tumours of the inner ear nerve that can be observed or treated effectively with radiation or surgery. Tumours that are growing over time should receive treatment, of which radiation therapy (RT) is an effective option. Radiation therapy is a non-invasive method of treating acoustic neuromas. Radiotherapy relies on high-energy x-rays that penetrate the head and skull to target the tumour while avoiding surrounding normal body structures. These x-rays damage the DNA of the tumour cells, causing them to stop growing. There are two main methods to deliver RT for acoustic neuromas, stereotactic radiosurgery (SRS) or fractionated irradiation.
What is stereotactic radiosurgery (SRS)?
SRS is defined by the use of a single, high-dose treatment aimed at a target in the head. SRS typically relies on the use of a rigid, stereotactic frame that is anchored to the outside of the skull using three or four metal pins (Figure 1). The stereotactic frame is a piece of hardware that reduces the patient’s head movement to ensure a very high precision of treatment.
SRS can be delivered through a number of technologies, including cobalt-based systems (also known as Gamma Knife, Perfexion, or Icon), CyberKnife, or a linear accelerator (trade names include, but are not limited to, RapidArc, TrueBeam, Versa). SRS is prescribed by a radiation oncologist and a neurosurgeon, who work closely with a physics and therapist team.

A typical workflow is as follows: A patient undergoing SRS obtains a high-resolution MRI and CT of their tumour. The stereotactic frame is applied by a neurosurgeon on the morning of the treatment with local anesthetic (freezing) at the pin sites. A dedicated team consisting of a medical physicist, neurosurgeon, radiation oncologist, and therapists create a personalized radiation plan. The frame (and the patient) is docked to the radiation machine, and the treatment begins. Treatment length can range from 20 -120 minutes. After treatment, the frame is removed, and the patient is taken home the same day by a companion.
What is fractionated radiotherapy?
The term “fractionated” refers to the fact that this form of radiation is delivered over a course of 25-30 treatments (5-6 weeks). Fractionated radiation is almost always delivered using a linear accelerator. Patients are immobilized using a plastic mask, so a stereotactic frame is not necessary. Each daily treatment takes 5 -15 minutes per day, and patients can attend outpatient appointments at the cancer centre unaccompanied. Patients typically feel well before and after treatments and can continue normal daily activities without restrictions.
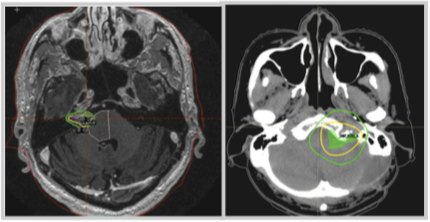
Figure 2. Green lines show moderate radiation dose, whereas yellow lines show high radiation dose. (Left) Stereotactic radiosurgery (gamma knife/Perfexion) plan. (Right) Fractionated radiation plan (linear accelerator). Image credit: D. Tsang
How to choose between radiation treatments?
Factors that affect the choice between radiation treatment type include the tumour size and availability of SRS. In patients with small tumours, SRS offers a more focused, precise radiation plan. This is because the method of immobilization for SRS is more rigid through use of a stereotactic frame. SRS is very precise, which reduces the volume of normal brain tissues that receive a low-to-moderate dose of radiation (Figure 2).
For larger tumours, SRS is not feasible because a single high dose of radiation can cause more side effects in the setting of a large treatment volume. Thus, larger tumours are usually referred for surgery or fractionated irradiation.
How effective is radiation therapy?
Both SRS and fractionated radiation work very well, with long-term tumour control rates greater than 90%. Both treatments work equally well at controlling acoustic neuromas.
For more statistics, visit:
Article by Lo et al. 2018: https://doi.org/10.1016/j.ijrobp.2017.09.024Article by Persson et al. 2017: https://dx.doi.org/10.1007/s00701-017-3164-6
What are some side effects of radiation therapy?
These can include: fatigue, headache, rash, hair loss (partial), hearing loss and ringing in the ears (tinnitus). Very rarely, patients can get seizures, facial weakness or numbness, brain swelling/ normal pressure hydrocephalus, or other brain tumours after radiation treatment. The risk of hearing loss, facial weakness or facial numbness does not differ between SRS or fractionated radiation.
How does radiation differ from surgery?
Surgery is sometimes preferred for patients with large tumours, tumours that are pushing on surrounding organs (brain or brainstem), patients with symptoms, those whose hearing may already be lost, or younger patients. Radiation is sometimes preferred for patients with intact hearing, smaller tumours, or for whom surgery is not possible or safe (due to other medical conditions).
The recovery from surgery takes longer (in the range of many weeks), whereas the recovery from radiation is shorter (in the range of a short number of days). There is no one factor that predisposes one to choose a specific treatment over another. Patients should speak with their doctors to discuss what is best for them.
What is the follow-up plan after radiation?
Because acoustic neuromas are very slow-growing tumours, they do not always shrink after radiation. In fact, some acoustic neuromas swell slightly after treatment, and then stop growing or shrink over time. The goal of the treatment is to stop the tumour from growing. Most tumours remain stable after time, without any growth or shrinkage. A minority will shrink slightly with time, over the course of many years.
After radiation treatment, your doctor will usually arrange for a follow-up MRI and clinic visit 6 months after treatment, then annually. After 5 years, your follow-up will stretch out to every 2 years. After 10 years, you may be discharged from follow-up, or receive MRIs every 2-3 years. Your doctor may order audiograms to check your hearing and offer hearing aids if needed.
If you have any questions about whether radiation is a suitable treatment for your acoustic neuroma, contact your doctor and ask her or him about this option.

Dr. Derek Tsang, MSc, MD, FRCSC is a fellowship-trained and board-certified radiation oncologist. He is an Assistant Professor of Radiation Oncology at the University Toronto. Dr. Tsang works at Princess Margaret Cancer Centre and Toronto Western Hospital at University Health Network in Toronto and at the Hospital for Sick Children. He holds a Master’s degree in clinical epidemiology from the Harvard T.H. Chan School of Public Health. Dr. Tsang treats primary central nervous system and paediatric tumours.

Nasim Sarhan, MD. Having graduated in Jordan in 2010, Dr. Sarhan undertook specialty training in radiation oncology at King Hussein Cancer Center where he was a consultant for three years. He currently is doing his fellowship at PMH in CNS, Stereotactic Radiosurgery and paediatric tumours.
